Glucose Transporters: SGLT Inhibitors and GLUT4 in Diabetes Management
This post explores the key roles of key glucose transporters, SGLTs and GLUT4, in glucose homeostasis and their implications for diabetes management. A thorough understanding of these transporters can provide valuable insights into the development of targeted therapeutic interventions.
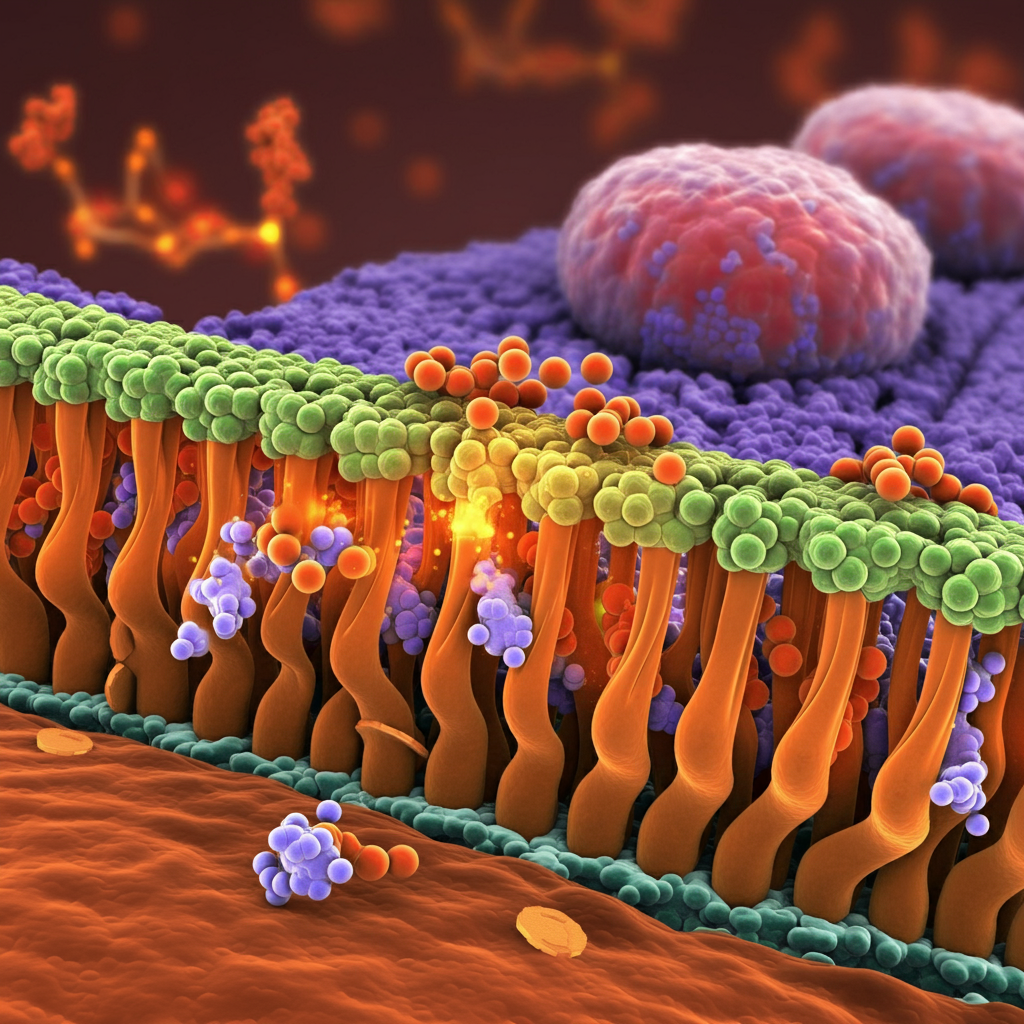
Cardiometabolic diseases, particularly diabetes and cardiovascular disease (CVD), constitute a major public health concern globally. The prevalence of these conditions has been steadily increasing, with a more rapid rise observed in middle- and low-income countries. Effective management of diabetes hinges on understanding the mechanisms involved in regulating glucose in the body. Central to this process are glucose transporters, proteins that facilitate glucose movement across cell membranes.
SGLTs: Guardians of Glucose Absorption and Reabsorption
Sodium-glucose cotransporters, or SGLTs, are primarily found in the intestines and kidneys, where they play crucial roles in glucose absorption and reabsorption, respectively. In the intestines, SGLTs mediate the uptake of glucose from the diet into the bloodstream. Subsequently, in the kidneys, SGLTs reclaim glucose from the glomerular filtrate, preventing its loss in urine.
These transporters are sodium-dependent and insulin-independent, meaning their function depends on the sodium concentration gradient across cell membranes and is not directly regulated by insulin.
Phloridzin: A Potential SGLT Inhibitor for Diabetes Management

Research highlights phloridzin as a potentially valuable therapeutic agent for managing hyperglycemia symptoms. The apple polyphenol is a potent and specific inhibitor of SGLTs. Phloridzin competitively and specifically binds to SGLTs, preventing glucose binding and transport. The inhibition reduces renal glucose reabsorption, resulting in increased glucose excretion in the urine and therefore a decrease in blood glucose levels.
Scientific publications note that phloridzin is a potential therapeutic agent for hyperglycaemia management in diabetes. It may reduce the required exogenous insulin dosage in Type 1 diabetes and improve blood sugar regulation in Type 2 diabetes. Visit the The review highlights the need for further research to establish the optimal vitamin D levels for different health outcomes, the impact of supplementation in individuals with varying vitamin D statuses, and the long-term effects of supplementation on chronic disease risks. Visit the IHP Mastery Program to learn more about phloridzin and its therapeutic effects.
GLUT4: The Insulin-Sensitive Glucose Gatekeeper
In contrast to SGLTs, GLUT4 is an insulin-dependent glucose transporter found predominantly in skeletal muscle, adipose tissue, and the heart. These tissues have high glucose demands and rely heavily on insulin-stimulated glucose uptake for energy production and metabolic functions.
The binding of insulin to its receptors on the cell surface initiates a signalling cascade that results in the translocation of GLUT4 transporters from intracellular vesicles to the cell membrane. This increased GLUT4 presence on the cell surface facilitates glucose uptake into the cells.
Insulin Resistance and GLUT4 Dysfunction in Diabetes
The insulin-dependent nature of GLUT4 makes the primary locations (skeletal muscle, adipose tissue, and the heart) particularly susceptible to the detrimental effects of insulin resistance and low insulin levels, as observed in diabetic patients. In such conditions, insulin’s ability to stimulate GLUT4 translocation and subsequent glucose uptake is compromised, leading to elevated blood glucose levels.
EGCG: A Potential Alternative Pathway for Diabetes Management
EGCG (epigallocatechin gallate) is a major polyphenol found in green tea. It is known for its potential to help manage diabetes by promoting glucose uptake in muscle cells, even when insulin signalling is weak.

EGCG helps muscle cells absorb glucose, and one of the primary ways EGCG helps with diabetes is by promoting GLUT4 translocation in skeletal muscle. Skeletal muscle is a major site for glucose utilisation in the body. EGCG helps move GLUT4 to the muscle cell surface, making it easier for glucose to enter, even when insulin signalling is weak.
Another key factor to note, EGCG works differently than insulin. Insulin plays a crucial role in regulating blood sugar levels by instructing cells to take up glucose. However, in type-2 diabetes, cells become resistant to insulin’s signals, leading to high blood sugar. EGCG, unlike insulin, appears to stimulate GLUT4 translocation through a different pathway that doesn’t rely on insulin. This means EGCG may still be effective in lowering blood glucose even when insulin is not working correctly.
In this way, EGCG may help improve blood sugar control, especially in people with diabetes who have difficulty responding to insulin.
SGLTs and GLUT4: Distinct Transporters, Different Therapeutic Avenues
Understanding the distinct roles of SGLTs and GLUT4 in glucose transport is crucial for developing targeted therapeutic strategies for diabetes management. While both transporters are essential for maintaining glucose homeostasis, they differ in their tissue distribution, mechanisms of action, and regulatory factors.
In addition to phloridzin and EGCG, other nutritional supplements and botanicals show promise in modulating glucose transporter activity.
For example:
- Berberine: Activates AMP kinase, increasing glucose uptake and reducing blood sugar.
- Chromium: Regulates blood sugar, inhibits excessive insulin cross-linking, and improves glucose uptake, potentially reducing insulin resistance.
- Gymnema Sylvestre: Contains compounds that stimulate insulin secretion and delay glucose absorption from the blood.
- White Mulberry Leaf: Slows the breakdown of sugars in the gut, promoting gradual absorption into the bloodstream and aiding in blood sugar control.
A Holistic Approach to Diabetes Care
The management of diabetes extends beyond glucose control and necessitates a multifaceted approach that encompasses lifestyle modifications, dietary interventions, and targeted nutritional supplementation.
By understanding the complexities of glucose transporters like SGLTs and GLUT4, medical professionals can develop more effective and personalised treatment plans for their patients. Further research is needed to fully elucidate the therapeutic potential of modulating these transporters for managing diabetes and other glucose-related disorders.
How do I Become a Functional Medicine Practitioner to learn more about Glucose Transporters?

The Institute of Integrative Medicine is a global leader in the field of Integrative Medicine Education. Integrative medicine aims to be at the forefront of modern technology and new discoveries and focuses on the root cause of disease. Effective management of diabetes depends on understanding the mechanisms involved in regulating glucose in the body. Understanding these transporters may provide insights into applying targeted therapeutic interventions. We offer certified online courses helping you to take charge of your practice and improve the quality of life for your patients. Find out more about the courses we offer today!

