Obesity and Asthma Comorbidity
Obesity and asthma, two seemingly separate conditions, are increasingly recognised as intertwined. Chronic inflammation, fuelled by changes in adipose tissue and its signalling molecules, acts as a bridge between these conditions. Understanding this inflammatory connection is crucial for physicians to effectively manage both obesity and asthma, leading to improved patient outcomes.
Obesity and asthma, two prevalent health challenges in the developed world, are increasingly recognised as interconnected. Although seemingly distinct, a growing body of evidence reveals a complex and concerning link between these two conditions, driven by inflammation – a natural process that, when chronically dysregulated, may have far-reaching health consequences.
Understanding the Inflammatory Players
To grasp the intricate relationship between obesity and asthma, it’s crucial to understand the key inflammatory players involved.
1. Adipose Tissue
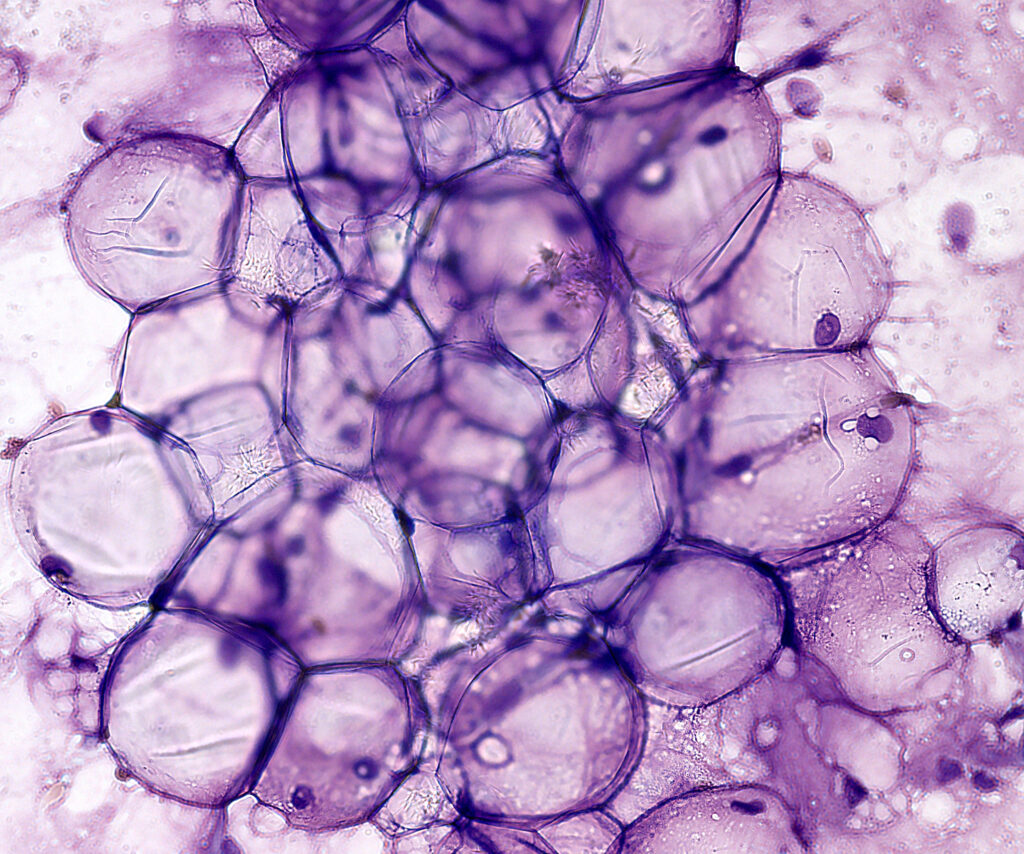
Adipose tissue (AT), or body fat, plays a much more active role in our health than previously understood. In cases of obesity, AT undergoes significant changes, becoming infiltrated with pro-inflammatory immune cells called macrophages, particularly M1 macrophages. These macrophages, along with enlarged fat cells (adipocytes), release a cocktail of inflammatory molecules called cytokines, including IL-6, TNF-α, and IL-1β. This chronic, low-grade inflammation in AT is termed “metainflammation.”
2. Adipokines
Adding another layer of complexity, AT also secretes signalling proteins known as adipokines, which act as messengers throughout the body. Two key adipokines are central to the obesity-asthma link:
- Leptin: Often called the “satiety hormone,” leptin helps regulate appetite and energy expenditure. However, in obesity, leptin levels soar, and the body develops leptin resistance, leading to a continued imbalance in energy intake and expenditure. Furthermore, leptin exerts pro-inflammatory effects, further contributing to the inflammatory milieu by stimulating the production of even more inflammatory cytokines, including TNF-α, IL-6, and MCP-1.
- Adiponectin: In contrast to leptin, adiponectin acts as an anti-inflammatory agent, countering the effects of pro-inflammatory cytokines and promoting insulin sensitivity. However, in obesity, adiponectin levels plummet, tilting the scales further towards inflammation. Research indicates that lower adiponectin levels are associated with a higher incidence of asthma in adults, highlighting its protective role.
3. NLRP3 Inflammasome
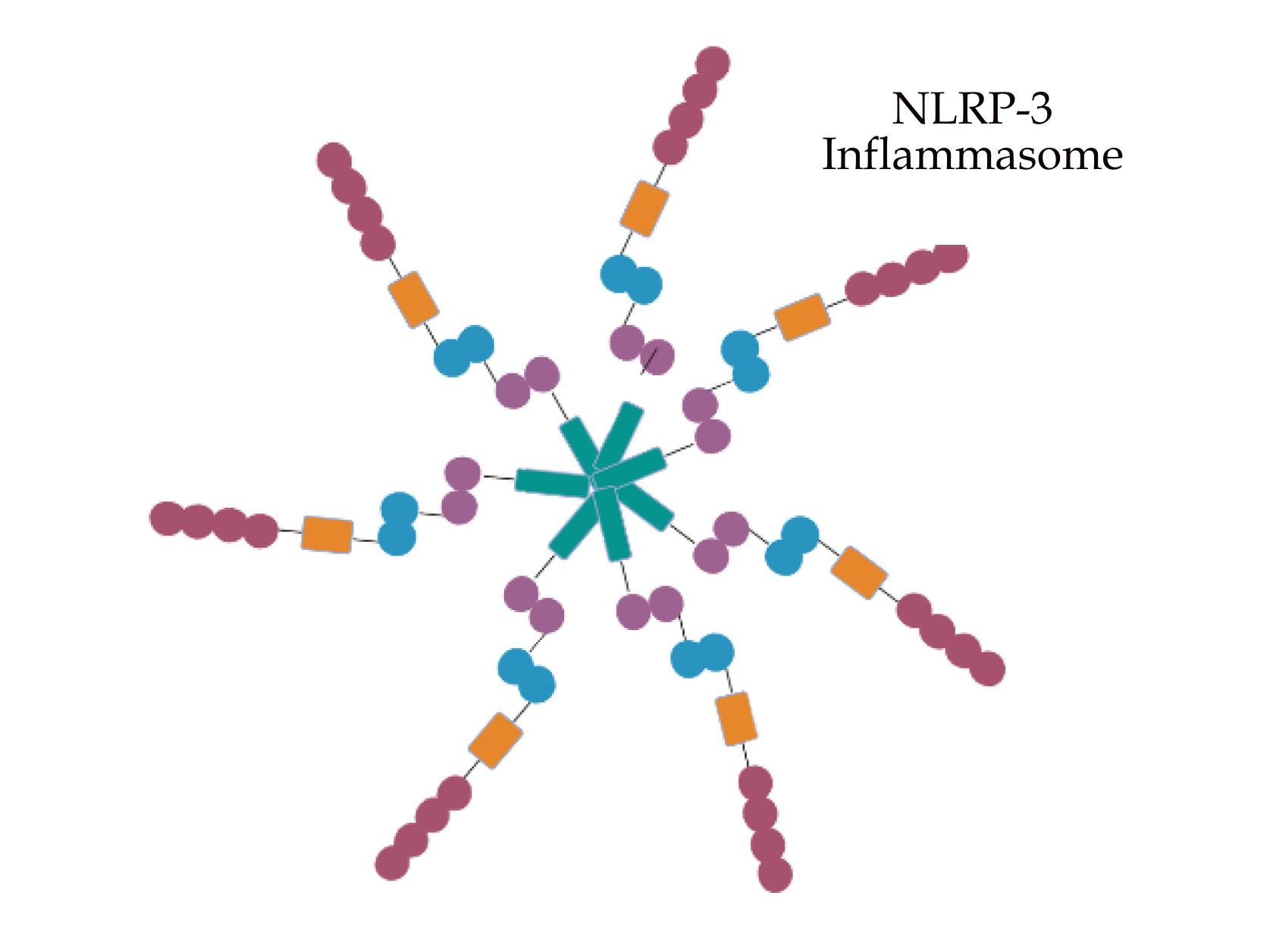
The NLRP3 inflammasome is a multiprotein complex found within cells that plays a crucial role in our immune response. When activated, it triggers the release of inflammatory cytokines, particularly IL-1β. In the context of obesity, factors such as saturated fatty acids and cholesterol crystals can activate the NLRP3 inflammasome, contributing to the chronic inflammation seen in AT.
Obesity and Asthma: Bridging the Gap Through Inflammation
So, how do these inflammatory players connect obesity and asthma?
- Shifting Immune Landscape: Obesity disrupts the balance of immune cells within AT, leading to an increase in neutrophils (immune cells associated with inflammation) and a decrease in eosinophils. This shift towards neutrophilic inflammation is mirrored in the airways of patients with obesity-associated asthma. This represents a departure from the typical eosinophilic inflammation seen in many other forms of asthma.
The inflammatory links between obesity and asthma underscore the critical importance of weight management in mitigating asthma severity and improving overall health. Studies have shown that even modest weight loss, achieved through lifestyle modifications such as diet and exercise, can have significant benefits for individuals with asthma. Weight loss helps to reduce AT inflammation, improve leptin sensitivity, and increase adiponectin levels, all of which contribute to a less inflamed and more balanced internal environment. To learn more about Obesity pathology and the integrative approach, take a look at the IHP Mastery Program.
- Amplified Airway Hyperresponsiveness: One of the hallmarks of asthma is airway hyperresponsiveness (AHR), where the airways are overly sensitive to triggers like allergens, irritants, or even cold air. Leptin, with its pro-inflammatory nature, appears to exacerbate AHR, creating a scenario where the airways become even more reactive and prone to constriction. This may explain why individuals with obesity often experience more severe asthma symptoms.
- Shared Inflammatory Pathways: Research suggests that activation of the NLRP3 inflammasome may provide a direct link between obesity and asthma. In obesity, the NLRP3 inflammasome becomes activated not only in AT but also in the lungs. This activation leads to a surge in IL-1β, which in turn activates another type of immune cell called ILC3. These ILC3 cells release IL-17A, a cytokine known to promote airway inflammation and AHR.
The Importance of Weight Management
Beyond the Scale: A Holistic Approach to Care

Addressing the complex interplay between obesity and asthma requires a multifaceted approach. Physicians and other healthcare providers should consider the potential role of obesity in asthma management and vice versa. This includes:
- Recognising the Distinct Phenotypes: Understanding the two main asthma phenotypes associated with obesity — early-onset in children and late-onset in adults — is crucial for tailoring treatment plans.
- Evaluating Inflammatory Markers: Monitoring inflammatory markers, including leptin, adiponectin, and IL-6, can provide valuable insights into disease severity and guide treatment decisions.
- Prioritising Weight Management: Encouraging and supporting weight loss through lifestyle changes, and in some cases, bariatric surgery, is crucial for improving asthma control and overall well-being.
- Addressing Metabolic Health: Evaluating and managing metabolic health, including factors such as insulin resistance and blood sugar levels, is important for all asthmatic patients, not just those with obesity.
The Path Forward
While significant strides have been made in understanding the inflammatory mechanisms linking obesity and asthma, much remains to be explored. Continued research is vital to unravel the intricate web of interactions between these conditions. Collaborative efforts between researchers, healthcare providers, and public health initiatives are crucial to translate scientific discoveries into effective strategies for prevention, early intervention, and improved patient care. Specifically, future research should focus on:
- Identifying novel therapeutic targets to disrupt the inflammatory pathways linking obesity and asthma
- Developing personalised treatment approaches based on individual patient characteristics and disease phenotypes
- Implementing comprehensive public health interventions to address the root causes of obesity and asthma
By fostering collaboration and innovation, we’re able to pave the way for a future where the burden of these chronic conditions is significantly reduced, leading to improved quality of life for countless individuals.
How do I Become a Functional Medicine Practitioner to learn more about the Asthma-Obesity Link?

The Institute of Integrative Medicine is a global leader in the field of Integrative Medicine Education. Integrative medicine aims to be at the forefront of modern technology and new discoveries and focuses on the root cause of disease. Obesity and asthma, two seemingly disparate conditions, are intricately linked through a web of inflammatory processes. Understanding these mechanisms is crucial for physicians to effectively manage both conditions and improve patient outcomes. The IHP program addresses this critical need by equipping healthcare professionals with the knowledge to confidently utilise these interventions. We offer certified online courses helping you to take charge of your practice and improve the quality of life for your patients. Find out more about the courses we offer today!

