Pharmacogenomics: 6 Benefits of personalised medicine
In a 1994 study on hospitalised patients, it was shown that negative drug reactions led to approximately 100 000 deaths (Journal of the American Medical Association, 1994). This is a demonstration on the risks associated with unclear drug prescriptions. The rate of successful drug metabolism is dependent on a person’s genomic structure. Pharmacogenomics is fairly…
In a 1994 study on hospitalised patients, it was shown that negative drug reactions led to approximately 100 000 deaths (Journal of the American Medical Association, 1994). This is a demonstration on the risks associated with unclear drug prescriptions. The rate of successful drug metabolism is dependent on a person’s genomic structure. Pharmacogenomics is fairly young in its inception, but has made headway in the approach to personalised medicine.
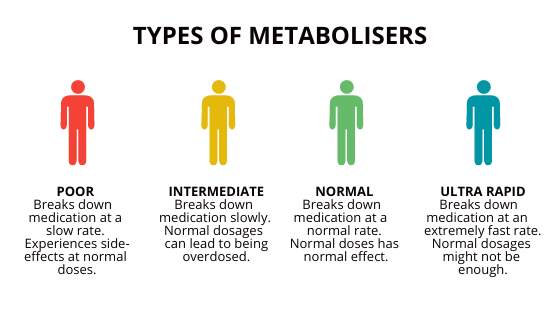
The CYP450 enzyme controls the breakdown of around 30 different categories of drugs (Journal of Clinical Medicine Research, 2009). In previous articles, we’ve looked at the very basis of genetics, which bodes well for understanding the influence DNA has on our ability to metabolise drugs. DNA variations in our genes that code for these liver enzymes, can determine our reaction to certain medications (Figure 1). Thus, it is important to understand how personalised medication works and why it is beneficial to clinicians and health specialists alike.
Benefits of Pharmacogenomics
Vaccine refinement
The year 2020 was one of the most chaotic years our generation has seen. Amongst a plethora of political and social unrest, a viral pandemic is really what brought the world to a stand still. Such a giant of its time has only now begun to ease its effects, thanks to the progress in vaccine production and rollout.
Vaccines that consist of genetic material (DNA, RNA) will help in lowering risk by activating the immune response without causing infection. This method of vaccine creation is far more cost effective and practical.
Accurate drug dosage
Soon, the days of evaluating dosage based on weight and age will be over. Studying your patient’s DNA gives great insight into how well the body processes the medication, as well as the time frame in which it takes to metabolise. Essentially, this will help lower the risk of under or overdosing.
Advanced lifestyle modification
Insight into DNA aids in the ability to predict the onset of disease, meaning the patient is able to catch this at an early stage. With this in mind, one is able to make suitable lifestyle modifications to help delay or prevent the onset of these diseases or health issues. One is also able to monitor disease more effectively, in order to treat at the earliest and most important stages.
Cheaper health care
There is a lot that goes into the evaluation of a drug. By individualising patient care through genomic insight, companies (as well as patients) are able to minimise their costs on potential drug failure. For example, a patient may spend a large amount of money on a drug for 6 months, that is doing nothing for them. Secondly, understanding our genetic history and function allows us to catch the onset of disease at its fundamental stages, lowering the cost it would have if potentially caught at the later stage.
Safer drug prescription
As mentioned above, a patient could wait months before finding the right medication. This costs time and money, but also affects the health status of the patient. Instead of using a method of “trial-and-error”, a clinician is able to analyse their patient’s genome and prescribe accordingly. Thus, limiting the time and money it costs to prescribe the right medication.
More effective medication
By basing pharmaceutical creation on DNA and RNA, companies can effectively facilitate drug discovery. With this knowledge and pharmacogenomics, scientists are able to produce more centralised drugs to treat specific diseases and viruses. In doing this, vaccines become more effective and the risk of cell damage is far less.
Summary
Pharmacogenomics is still in its infancy, but is providing scientists and clinicians with the tools they need to provide more effective healthcare. For a very long time in history, people have faced the burdens of ineffective medical treatment. This is where integrative healthcare approaches are filling in the gaps. As science advances, and technology allows us better insight into our physiology, the future of medicine looks brighter. To personalise medicine is to make each person’s needs a top priority, building better relationships between our healthcare specialists and their patients.
How do I Become a Functional Medicine Practitioner to learn more about Pharmacogenomics?

The Institute of Integrative Medicine is a global leader in the field of Integrative Medicine Education. Integrative medicine aims to be at the forefront of modern technology and new discoveries and focuses on the root cause of disease. The field of pharmacogenomics offers a powerful tool to personalise medication use for your patients. By analysing individual genetic variations, you can identify how they metabolise drugs, allowing for targeted dosing and reduced side effects. This translates to improved efficacy, minimised adverse reactions, and ultimately, better patient outcomes. Integrative medicine strengthens this approach by providing a holistic view of your patients’ health. We offer certified online courses helping you to take charge of your practice and improve the quality of life for your patients. Find out more about the courses we offer today!

