The Gut Connection – How Microbiome Modulation Influences Cancer Risk
The gut microbiome, once a silent observer, now takes centre stage in the cancer conundrum. Dysbiosis, its discordant note, can lead to disease progression. Modulating the microbiome holds immense potential for prevention and personalised treatment. Imagine wielding prebiotics and probiotics as tools, conducting individuals towards gut health harmony. This is not a distant dream, but a burgeoning field poised to rewrite the cancer narrative, one modulated microbe at a time.
You are what you eat – a proverb that holds more truth than we realise. Food not only nourishes our bodies, it also feeds a hidden world within us: the gut microbiome. This vast and diverse community of microorganisms, primarily bacteria, resides in our intestines and is essential to overall health and well-being.

These little residents influence far more than digestion alone. They shape our immune system, metabolism, and even mental state. A healthy gut microbiome is rich with beneficial bacteria that aid in nutrient absorption, fight harmful pathogens, and produce essential vitamins and compounds. However, an imbalance in this delicate ecosystem, known as dysbiosis, can result in digestive disorders, inflammatory conditions, chronic diseases and even cancer.
Understanding the profound impact of the gut microbiome on our health opens promising possibilities for disease prevention in conjunction with integrative medicine. By nurturing this internal ecosystem through dietary choices, probiotic supplementation, and other lifestyle modifications, we can empower gut microbes to work their magic and unlock an increased level of well-being.
Demystifying the Microbiome – A Thriving Universe Within:
Imagine a city with thousands of residents connected by a complex network. This isn’t a city of humans, but rather the microscopic world dwelling within your gut – the gut microbiome. Composed of primarily bacteria, with archaea, fungi, and viruses also present, this diverse community harbours an estimated 100 trillion microorganisms.
While the exact composition varies between individuals, the four main phyla of bacteria typically dominate:
- Bacteroidetes: Excel at breaking down complex carbohydrates and producing beneficial short-chain fatty acids (SCFAs) that nourish gut cells and regulate inflammation – often associated with a plant-based diet .
- Firmicutes: Includes many fibre-fermenting bacteria, as well as some that perform less favoured functions, like producing proinflammatory molecules.
- Actinobacteria: Contribute to immune function and break down dietary fibres.
- Proteobacteria: Some members of this phylum can be harmful, while others play roles in digestion and vitamin production.
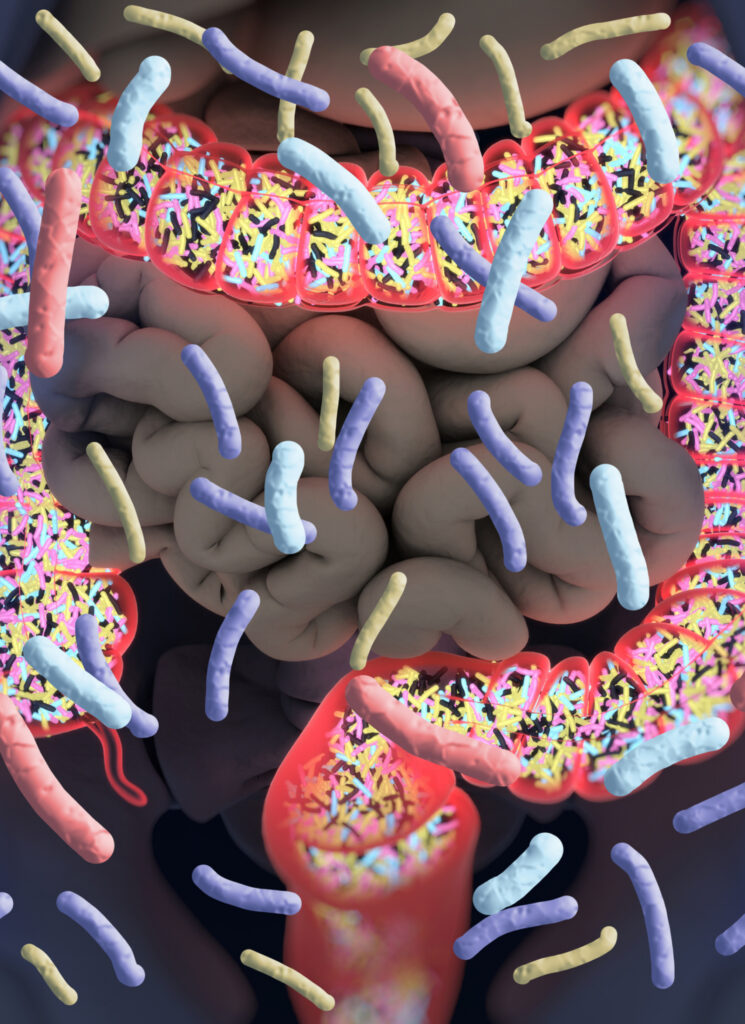
Beyond their individual contributions, gut microbes engage in complex interactions, creating a dynamic ecosystem with multifaceted functions. Some key roles include:
- Food Digestion: Microbes break down complex carbohydrates and produce essential nutrients our bodies cannot synthesise on their own.
- Modulating the immune system: The gut microbiome educates and trains the immune system, helping it differentiate between friend and foe.
- Producing beneficial metabolites: SCFAs from fibre fermentation not only nourish gut cells but also signal to distant organs, influencing metabolism and overall health.
- Protecting against pathogens: Beneficial microbes create a physical barrier and produce antimicrobial compounds that inhibit harmful invaders.
The Microbiome and Cancer – A Complex Interplay:
The intricate dance between the gut microbiome and cancer has captivated researchers in recent years. This multifaceted interplay involves a complex web of interactions. In particular, imbalances within the gut microbial community are increasingly recognised as a potential player in cancer development and progression.
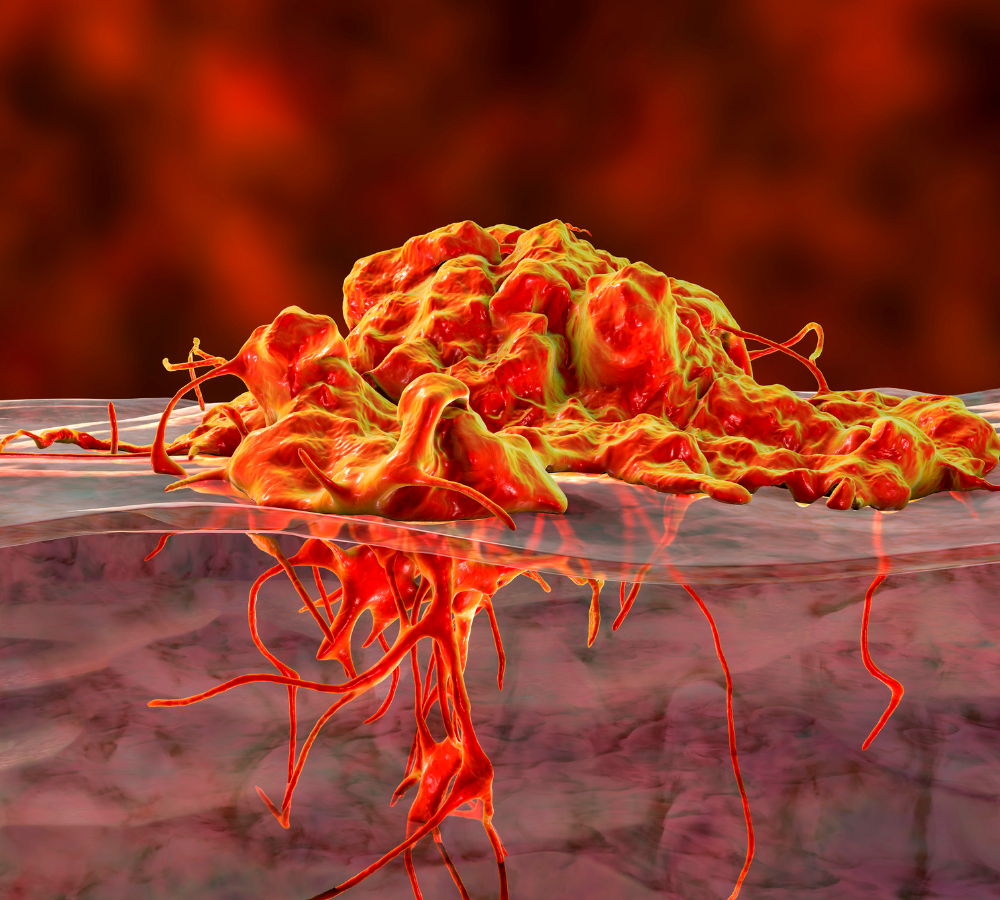
Emerging evidence suggests that specific microbial metabolites, inflammatory pathways, and altered immune responses due to a disrupted microbiome may contribute to oncogenesis across various cancer types. While the exact mechanisms remain under active investigation, understanding this intricate interplay holds immense promise for the development of novel preventative and therapeutic strategies aimed at modulating the gut microbiome for improved cancer outcomes.
Mechanisms Linking Gut Dysbiosis and Cancer Risk:
- Inflammation: Dysbiosis may trigger chronic low-grade inflammation, a known risk factor for cancer. Pro-inflammatory bacteria release toxins and activate immune cells, creating a pro-inflammatory environment that damages healthy tissues and fuels tumour growth. Disrupted gut barrier function in dysbiosis allows harmful bacteria and their products to leak into the bloodstream, further promoting systemic inflammation.
- Genotoxicity: Certain bacteria associated with dysbiosis produce genotoxins, like reactive oxygen species and DNA-damaging metabolites, that can directly damage the genetic material of healthy cells, increasing the risk of mutations and tumour initiation. Imbalances also alter the gut’s ability to detoxify harmful compounds, leading to higher exposure to carcinogens from food or the environment.
- Metabolic Alterations: Gut microbiota regulate various metabolic pathways. Dysbiosis can lead to imbalances in nutrient absorption, energy metabolism, and short-chain fatty acid production, leading to altered cellular signalling and tumorigenesis promotion. Some bacteria associated with dysbiosis can convert dietary components into potentially harmful metabolites that act as pro-carcinogens or promote cancer cell proliferation.
By understanding the intricate link between gut dysbiosis and cancer risk, we can harness the power of dietary choices to orchestrate a transformative “microbiome makeover,” potentially mitigating cancer risk and fostering overall well-being.
Dietary Choices for a Microbiome Makeover
As we delve deeper into the link between gut dysbiosis and cancer risk, the power of dietary choices to modulate the internal ecosystem becomes increasingly evident. Here are some specific dietary recommendations to orchestrate a “microbiome makeover”:
- Embrace Fibre Power: Fibre acts as prebiotic fuel for your gut microbes. Prioritise whole grains (brown rice, quinoa), legumes (beans, lentils), fruits, and vegetables, aiming for at least 25-35 grams of fibre daily – Fibre diversity is key, and go slow on the fibre increase.
- Minimise Processed Foods: Processed products have a reputation for being a cancer triggering food. These items are often stripped of fibre and packed with refined sugars, unhealthy fats, and additives. These can upset the gut microbiome’s delicate balance. Limit sugary drinks, refined carbohydrates (white bread, pasta), and processed meats.

- Introduce Fermented Foods: Fermented foods like yoghurt, kimchi, sauerkraut, and kombucha are rich in probiotics, live bacteria that contribute to a healthy gut ecosystem. Probiotics fight harmful bacteria and support immune function. Choose fermented foods with live and active cultures, and explore a variety to maximise benefits.
- Consider prebiotic supplements: Prebiotics, like inulin or oligosaccharides, can directly feed your gut microbes.
- Cancer Vegetarian Diet: In the fight against cancer, oncology and nutrition join forces, wielding personalised dietary strategies to bolster patients’ defences, manage side effects, and potentially lower cancer risk. A vegetarian diet, rich in fibre and diverse plant compounds, may help gut bacteria flourish and offer health benefits. Research has recently revealed that these diets may decrease the risk of specific cancer types – prostate cancer and colorectal cancer risk among men. In the case of postmenopausal breast cancer, the protective effect may be indirect through the modification of BMI. A detailed list of dietary recommendations for cancer types can be found in Module 12: Cancer of the IHP Program.
- Cancer raw food diet: Raw food diets emphasise uncooked, unprocessed, and organic foods. This diet has several benefits for cancer patients, including improved digestion, increased energy levels, and reduced inflammation. In addition to complementing conventional medical treatments, it may improve overall health.
Conclusion
We are still unravelling the intricate dance between the gut microbiome and cancer. By understanding the mechanisms linking dysbiosis to cancer risk and harnessing the power of dietary choices, prebiotics and probiotics, we are on the cusp of unlocking exciting frontiers in preventative and therapeutic strategies. While much remains to be discovered, the potential to personalise medicine and empower individuals to take charge of their gut health through lifestyle modifications offers a beacon of hope. In the long run, this will pave the way for a future where microbiome modulation improves overall health, reduces cancer risk, and leads to a brighter outlook.
How do I Become a Functional Medicine Practitioner to learn more about The Microbiome and Cancer?

The Institute of Integrative Medicine is a global leader in the field of Integrative Medicine Education. Integrative medicine aims to be at the forefront of modern technology and new discoveries and focuses on the root cause of disease. The gut microbiome, a universe of trillions of microorganisms, is no longer a hidden corner of human biology. Its influence on immune function and overall health is undeniable, and its potential role in cancer development demands exploration. Delving into this intricate link holds the key to unlocking personalised prevention strategies and improving patient outcomes. We offer certified online courses helping you to take charge of your practice and improve the quality of life for your patients. Find out more about the courses we offer today!

